- Agency for Health Care Administration
- Ascension
- Chad Poppel
- Chiquita Brooks-LaSur
- Dana Trabulsy
- Edward Forster
- Elizabeth Rochaine
- Florida Board of Medicine.
- Gregory Coffman
- John P. Fogarty
- Liz Dudek
- managed-care
- Matthew Benson
- Medicaid
- Nathan Landsbaum
- Robin Bartleman
- Ron DeSantis
- Shaddrick Hattson
- Veronica Catoe
- Wellington Regional Medical Center

Welcome back to Diagnosis, a vertical that focuses on the crossroads of health care policy and politics.
— Double dose —
As the opioid epidemic rages on, Florida receives another dose of State Opioid Response Grant funding to purchase overdose-reversing drugs that save lives.
The $120 million SOR infusion addresses unmet treatment needs and opioid overdose-related deaths through prevention, treatment, and recovery activities for opioid use disorder.
That includes purchasing overdose-reversal drugs, such as naloxone, a medication marketed under the Narcan brand.
However, potent synthetic opioids now account for the preponderance of overdose deaths in the state. According to Florida Department of Law Enforcement data, fentanyl — a compound 50 times more powerful than heroin — was responsible for 2,744 of the 3,959 opioid-related deaths (69%) reported last year.
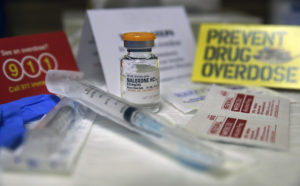
The potency of fentanyl and other synthetic opioids are testing the limitations of Narcan, typically administered in 4-milligram doses.
A recent study shows that two or more doses were needed in 78% of overdose treatment events where 4 mg Narcan was administered. In 30% of cases, it took three or more doses. The study also found that 86% of participants reported more confidence in an 8 mg naloxone nasal spray versus a 4 mg naloxone nasal spray.
Notably, for the third round of SOR funding, the federal government explicitly allows states to purchase a more powerful naloxone nasal spray, Kloxxado, which contains 8 mg of naloxone — double the amount found in Narcan.
According to Florida’s plan for the SOR funding, which the Department of Children and Families (DCF) administers, the state will prioritize widespread community saturation for any FDA-approved naloxone nasal spray. Previously, the plan only allowed for the 4 mg variant.
Law enforcement has been using Kloxxado to reverse overdoses for two years, shortly after it earned FDA approval. Advocates say every second matters when treating overdose patients and that Kloxxado provides the necessary dosage to combat the effects of increasingly powerful illicit drugs.
___
I welcome your feedback, questions and especially your tips. You can email me at [email protected] or call me at 850-251-2317.
— A closer look —
Often, one can get bogged down in all the numbers associated with Medicaid, the state’s safety net program that services the poor, elderly and disabled.
But let’s take a closer look at the most recent report related to what is known as “unwinding” or the process of trimming the rolls after the end of the COVID-19 national health emergency.
The June report says 75,327 were disenrolled from Medicaid and that of those disenrolled, 44,158 were “terminated for procedural reasons.” That translates to nearly 59%.

According to the report, the remaining 31,169 people were disenrolled because they did not meet eligibility requirements.
This breakdown is significant because those who keep tabs on Medicaid numbers in the states — including the federal government — have been concerned about how many people are removed for paperwork instead of no longer being eligible.
Meanwhile, a top-ranking Medicaid official told members of the Social Services Estimating Conference Committee last week that the Legislature anticipated higher disenrollment rates when crafting the Fiscal Year 2023-24 budget and, as a result, “We are over the budget by 245,000 people.”
— Seeking answers —
Has an adverse medical incident occurred if a surgically implanted device in a patient migrates from its original location?
What if the tip of an intentionally placed pain pump and epidural catheter breaks during a bedside removal, requiring the patient to undergo surgery to remove it? Did bedside health care trigger an adverse medical incident?
And how about if, during surgery, a drill bit broke and the surgeon who could not readily find and remove it decided it was safer to leave it in the patient? However, when the bit later “migrated to a different body surface,” posing a threat to the patient, it was surgically removed.

Is that an adverse event that requires reporting to the state?
Lee Moffitt Cancer & Research Institute does not think those three incidents, or five other similar instances, were adverse medical incidents that must be reported to the state.
But it wants to know for sure and has asked the state for its opinion.
The hospital petitioned the state for a declaratory statement “regarding whether certain events constitute a ‘procedure to remove unplanned foreign objects remaining from a surgical procedure’ that must be reported as an adverse incident.”
Florida law requires hospitals and ambulatory surgical centers to report specific adverse incidents to the state within 15 days of their occurrence. An adverse medical incident that: caused the patient to die or left the patient with a brain or spinal cord injury; required the transfer of the patient, within or outside the facility, to a unit providing a more acute level of care; a wrong surgical procedure, a wrong-site surgical procedure, or a surgical procedure otherwise unrelated to the patient’s diagnosis or medical condition. Additionally, adverse incidents include the surgical repair of damage resulting from a planned surgical procedure where the damage wasn’t an identified risk and a surgical procedure to remove unplanned foreign objects remaining from a surgical procedure.
In addition to the 15-day report, the law requires hospitals and ambulatory surgical centers to report adverse medical incidents annually. For the annual report, the definition of an adverse medical incident is also expanded to include events that caused the fracture or dislocation of bones or joints; resulted in a limitation of neurological, physical, or sensory function that continued after discharge from the facility; and any condition that following a planned surgery required specialized medical attention or surgical intervention without the patient’s informed consent.
— Tampa General expands —
Community Health Systems (CHS) announced Tuesday that it signed a definitive agreement to sell three facilities to Tampa General Hospital (TGH) and its affiliates for an estimated $290 million in cash.
The acquisitions give TGH a footprint in Hernando and Citrus counties.
“With this acquisition, TGH is not only expanding its geographic footprint to meet the needs of our state’s growing population, but TGH is also increasing access for Floridians to the world-class rare and complex specialized care we offer,” John Couris, TGH’s President and CEO, said in a published statement.

Tennessee-based CHS announced in a news release it would sell Bravera Health Brooksville, a 120-bed facility in Brooksville; Bravera Health Seven Rivers, a 128-bed facility in Crystal River; and Bravera Health Spring Hill, a 124-bed facility in Spring Hill and their associated assets to Tampa General Hospital and certain of its affiliates.
The transaction is expected to close later this year, subject to customary regulatory approvals and closing conditions.
— Knowledge is power —
Family members don’t often know about the resources available to people with developmental and intellectual disabilities. To diminish that problem, state Rep. Allison Tant championed legislation (HB 1517) during the 2023 Session that requires the Agency for Persons with Disabilities (APD) to convene an “interagency workgroup” and charged it with developing a “continuum of guidance” containing information that will help families better understand the education, workforce, daily living skills, and supportive services that are available to people throughout their life span.
APD has scheduled the meeting for 2:30 p.m. Aug. 2. While APD is directed by law to host the meeting, it will take place at DCF’s Tallahassee offices, located at 2415 N. Monroe St., Suite 400, Room C100, and not APD’s.

The law requires that, at a minimum, APD include representatives from AHCA, DCF, DOH, the Unique Employer Program at FloridaCommerce (formerly DEO), the Early Steps Program, the Department of Education’s Division of Vocational Rehabilitation, school district transition programs, Project 10, and the Florida Center for Students with Unique Abilities.
The law also clarifies that the interagency work group must identify the gaps in information and communication, determine why these gaps occur, and recommend ways to ensure that the data is more accessible. To do that, the interagency work group was directed to gather input from Florida families and other interested stakeholders.
APD must submit an interim report to the Governor and legislative leaders by Nov. 1. A final report is due Sept. 1, 2024.
— Women, Infants and Children —
The Department of Health seeks public input on improving the state’s Special Supplemental Nutrition Program for Women, Infants, and Children, commonly called WIC.
Ideas, comments and suggestions must be submitted by Aug. 31.

The U.S. Department of Agriculture funds WIC and serves low- to moderate-income pregnant, postpartum, and breastfeeding women and children up to age 5. The program provides a combination of nutritious foods, nutrition education, breastfeeding support, and referrals for health care.
Qualification is based on household income. A pregnant woman without children must earn $26,973 a year or less to qualify. For a family of three to qualify, annual income must be $45,991 or less. Income eligibility for a family of five is $65,009 a year or less.
According to the Florida Administrative Register notice, suggestions and comments should be emailed to [email protected]. Comments can be sent via fax to (850) 922-3936. Comments can also be sent by mail, attention Karen Martinez, Florida Department of Health, Bureau of WIC Program Services, BIN #A-16, 4052 Bald Cypress Way, Tallahassee, 32399-1726.
— RULES —
AHCA has published changes to proposed Rule changes 59B-12.001 regarding bone marrow transplantation. More here.
AHCA is amending Rule 59G-13.081 regarding the Developmental Disabilities Individual Budgeting Waiver Services Provider Rate Table. More here.
The Board of Chiropractic Medicine proposes amending Rule 64B2-13.007 regarding continuing education requirements during initial licensure periods. More here.
The Board of Chiropractic Medicine proposes amending Rule 64B2-13.004 regarding requirements for continuing education. More here.
The Council of Medical Physicists has published changes to proposed Rule 64B23-6.001 regarding penalty guidelines. More here.
The Office of Insurance Regulation (OIR) is proposing amending Rule 69O-238.001 regarding the application and renewal for pharmacy benefit managers. Email [email protected] or call (850) 413-4112 for a copy of the proposed rule.
OIR proposes amending Rules 69O-203.020, 69O-203.210, and 69O-203.215 regarding prepaid limited health service organization applications, discount plan organization applications and annual reports. More here.
OIR proposes amending Rules 69O-151.002, 69O-151.003, 69O-151.004, 69O-151.007, 69O-151.008, 69O-151.010, 69O-151.102, 69O-151.201, 69O-151.202, to update form references, remove duplicative language, update citations to the laws implemented, and make grammatical and stylistic changes to improve readability. It also proposes to delete Rules 69O-151.001, 69O-151.005, 69O-151.006, 69O-151.009, 69O-151.012, 69O-151.101, 69O-151.106, 69O-151.107. More here.
OIR proposes amending Rules 69O-137.001 and 69O-137.004 regarding annual and quarterly reporting requirements and required health insurer reporting, respectively. More here.
— LOBBYISTS —
Courtney Coppola, Ballard Partners: Trulieve
— ETC —
— NCCI released the Quarterly Economics Briefing (QEB) — Q2 2023. In this briefing, we examine economic indicators to assess the likelihood and shape of a potential recession. More here.
— University of Florida Health researchers have successfully removed and replaced a malfunctioning gene that gradually damages photoreceptors in the eye using what it describes in a news release as a type of “genetic scissors,” Working in mouse models, the researchers say the findings are a crucial step in developing a treatment for the disorder known as cone-rod dystrophy 6. More here.

— Joedrecka S. Brown Speights’ insights on physician mental health were published in the latest edition of Florida Family Physician. Speights, M.D., is a professor and chair of the FSU College of Medicine’s Department of Family Medicine and Rural Health.
— ROSTER —
— Paul DiGiorgi, M.D., has been named the incoming President of the Florida Society of Thoracic and Cardiovascular Surgeons. DiGiorgi has worked at Lee Health’s Shipley Cardiothoracic Center for 15 years.

— Kevin Andrews was named the next COO of Retreat Behavioral Health.
— William Walders was named Chief Information Officer for BayCare.
— Cory Mead was named CEO of HCA Florida Woodmont Hospital in Tamarac.
— David Vecchione, M.D., joined Spine & Orthopedic Center in Fort Lauderdale. He earned his medical degree from New York University School of Medicine and completed his residency at Jackson Memorial Hospital in Miami.
— Sergio Tierrablanca, D.O., joins Baptist Health as a family medicine physician. Tierrablanca completed his family medicine residency at Broward Health Medical Center. He earned his medical degree from the Nova Southeastern School of Osteopathic Medicine in 2020.
—ICYMI —
In case you missed them, here is a recap of other critical health care policy stories covered in Florida Politics this past week.
“Medicaid ‘unwinding’ not what state expected” via Christine Jordan Sexton of Florida Politics — The number of Floridians enrolled in the state’s health care safety net program is not dropping as much as anticipated. Even as state officials remove people from Medicaid rolls, thousands more than expected are enrolling in the safety net program. Florida started “unwinding” Medicaid with the end of the public health emergency caused by the COVID-19 pandemic. Florida health care officials anticipated about 900,000 people would be disenrolled from the program by the end of June. Agency for Health Care Administration (AHCA) Deputy Secretary of Health Care Finance Data Tom Wallace told the Social Services Estimating Conference that 640,000 people had been removed from the Medicaid program in the 12 weeks since the state started the “unwinding” process.

“Report: Medicaid enrollment dipped by 2% in June” via Christine Jordan Sexton of Florida Politics — The month of June saw about a 2% reduction in the number of residents enrolled in Medicaid, the health care safety net program for the elderly, poor and disabled. That’s a far smaller drop than what the DeSantis administration was expecting. A recently published report shows that as of June 30, 5,427,530 people enrolled in Medicaid as the state continues to “unwind” from the public health emergency (PHE). That figure includes 8,287 children enrolled in an optional Medicaid expansion program called MediKids.
“Lawyers push to make transgender care court challenge a class-action lawsuit” via Christine Jordan Sexton of Florida Politics — Those suing over Florida’s ban on gender-affirming care for minors want to expand the lawsuit to address restrictions on care against adults and widen the legal challenge into a class-action lawsuit. The amended complaint adds four adults who say they are facing disruptions in their medical care due to SB 254, the new law dealing with gender-affirming care passed by the Legislature and signed by DeSantis. Some of the other parts of the law, as well as the Board of Medicine and Board of Osteopathic Medicine rules that are being challenged, include a ban on advanced practice registered nurses from treating patients. The law also bans physicians and patients from using telehealth, requiring in-person consultation for all care.
— FOR YOUR RADAR —
Aside from coverage by Florida Politics, these stories are worth your time.
“Florida fights judge’s order to stop steering severely disabled kids into nursing homes” via Carol Marbin Miller of the Miami Herald — One week after a federal judge ordered Florida health administrators to cease relying on nursing homes for the care of children with complex medical needs, the state is back in court, arguing that it would be “impossible” to comply with the judge’s ruling. For more than a decade, lawyers for the state Agency for Health Care Administration fought a lawsuit by the U.S. Justice Department’s civil rights division that seeks to remove children, some just infants and toddlers, from nursing homes. The Justice Department claimed that Florida’s health policies, in effect, forced the parents of children with severe disabilities to institutionalize their children in violation of federal civil rights laws such as the Americans with Disabilities Act.
“Florida abortions top 38,000 in the first half of 2023 as six-week ban case hearing looms” via Brandon Girod of the Pensacola News Journal — Florida abortions in the first half of 2023 topped more than 38,000, according to the state Agency for Health Care Administration website, up from the 33,382 abortions performed in the first half of 2022. DeSantis signed a six-week abortion ban throughout Florida in April, but the new ban hasn’t taken effect yet as the state waits to see if its current 15-week ban is upheld in an ongoing legal battle before the state Supreme Court. The Florida Supreme Court is set to hear arguments in the case on Sept. 8. Should the court rule in favor of the ban, it would implement the state’s stricter six-week ban and determine whether a privacy clause in the Florida Constitution would protect abortion rights.

“Tampa General to buy three local hospitals from Tennessee company” via Shauna Muckle of the Tampa Bay Times — Tampa General Hospital has agreed to buy three Bravera Health hospitals north of Tampa for $290 million. Community Health Services, the current owner of the three Brooksville, Crystal River and Spring Hill hospitals, announced the sale. Once the deal closes, the Franklin, Tennessee-based company will no longer have any hospitals or clinics in Tampa Bay, leaving the operator with seven hospitals in the Panhandle, Southwest Florida and the Keys. In 2020, CHS sold St. Petersburg’s embattled Bayfront Health to Orlando Health. Since 2016, CHS has been shedding hospitals to focus on regional hubs, per a 2018 report from Healthcare Dive. The health care giant, which owns or leases 77 hospitals across 15 states, reported a $51 million net loss attributable to shareholders for the first quarter of 2023.
“Sarasota County responders to supply overdose-reversing drug” via the Venice Gondolier — Thanks to a state program, Sarasota County Fire Department (SCFD) emergency responders won’t just be able to treat an opioid overdose; they’ll be able to leave some of the overdose-reversing drugs behind. The Sarasota County Department of Health and Human Services and SCFD have joined the Helping Emergency Responders Obtain Support Program. Under it, SCFD can give a caregiver free naloxone as a precaution in case of a future overdose, a news release says. Naloxone reverses the effects of overdosing on medications such as heroin, oxycodone, fentanyl and morphine. It can restore breathing within two to three minutes. In 2022, SCFD responded to 844 drug overdoses and administered 1,087 doses of Naloxone, the release says.
“Orlando Health patients may lose UnitedHealthcare coverage amid stalled contract dispute” via Caroline Catherman of the Orlando Sentinel — Thousands of UnitedHealthcare members in Central Florida may soon lose access to in-network care at Orlando Health amid stalled contract negotiations. United’s contract with Orlando Health’s doctors and hospitals expires July 31, and if the two groups cannot reach an agreement before then, most services will no longer be covered for people on several plans. After months of negotiating new terms, with less than two weeks to go, both sides have accused the other of holding up negotiations, making misleading statements about the talks and making unreasonable proposals.
— PENCIL IT IN —
Thursday
9 a.m. — The Florida Board of Massage Therapy meets. Location: Holiday Inn Orlando-Disney Springs, 1805 Hotel Plaza Blvd., Lake Buena Vista.
9 a.m. — The Florida Board of Nursing Home Administrators meets. Holiday Inn Orlando-Disney Springs, 1805 Hotel Plaza Blvd., Lake Buena Vista.
10 a.m. — The Florida Chamber Foundation “Root Cause Matters: Addressing Justice to Tackle Florida Childhood Poverty.” More here.
1 p.m. — The Florida Boards of Medicine and Osteopathic Medicine Joint Anesthesiologist Assistant Committee meet. Join the virtual meeting from your computer, tablet, or smartphone here. Or call (571) 317-3112; participant code: 717632629.
Friday
Happy birthday to longtime (but never retired) reporter Bill Cotterell, former Agriculture Commissioner Adam Putnam and Florida Health Care Association Director of Communications Kristen Encizo Knapp.

9 a.m. — The Florida Board of Massage Therapy will meet. Holiday Inn Orlando-Disney Springs, 1805 Hotel Plaza Blvd., Lake Buena Vista.
Tuesday
Happy birthday to former state Sen. Garrett Richter and former state Rep. Jennifer Sullivan.
Wednesday
Happy birthday to Dean Cannon, President and CEO of GrayRobinson and former House Speaker, former St. Petersburg Mayor Rick Kriseman and Kevin Cate, founder of CATECOMM.
9 a.m. — The DOH Institutional Review Board meets to conduct and review new research studies involving human participants, modifications to existing studies, and continuing review of ongoing research to ensure research studies comply with regulations per the department’s ethical standards. 2585 Merchants Row Blvd., Conference Room 320P Tallahassee, Call (850) 245-4585 for a copy of the agenda.
2:30 p.m. — The Agency for Persons with Disabilities holds an interagency work group to improve communication and information for individuals applying for and receiving services.
___
Diagnosis is written by Christine Jordan Sexton and edited by Drew Wilson.