- Agency for Health Care Administration Secretary Mary Mayhew
- Andy Antenor
- Broward Health
- Center for Medicaid and CHIP Services
- Craig Waters
- Florida Covering Kids & Families
- Florida Gov. Ron DeSantis
- Florida Health Care Association
- Florida KidCare
- Florida Voices for the Unborn
- FoundCare
- Healthcare District of Palm Beach County
- Inc.
- Jodi Ray
- Marcia Young
- Medicaid
- Moffitt Cancer Center
- Molina Healthcare
- Paul Tanner
- Rep. Kathy Castor
- Rob Johnson
- Roe vs. Wade
- Sen. Ana Maria Rodriguez
- Simply Healthcare Plans
- Stacy Angier
- The Affordable Connectivity Program
- The Board of Nursing
- The Board of Nursing Home Administrators
- The Board of Pharmacy
- The Board Orthotists and Prosthetists
- The Mayernick Group
- University of Florida Health Cancer Center.
- University of Miami Sylvester Comprehensive Cancer Center
- Weesam Khoury
- West Cocoa Pharmacy and Compounding
Welcome back to Diagnosis, a vertical that focuses on the crossroads of health care policy and politics.
Memorial Day is just around the corner. It’s the kickoff of the Summer and the start of the countdown to a new fiscal year … and some budget vetoes.
It’s been more than two months since Florida legislators passed a $112 billion budget, but they still haven’t officially sent it to Gov. Ron DeSantis.
During that time, DeSantis has held numerous events around the state where he has announced his support for various hometown projects included in the spending plan as well as major items he recommended, like a $37 million boost in cancer research.

It’s not surprising that legislative leaders have held off sending the budget to DeSantis since the Governor has called not one, but two Special Sessions. Holding off on what budget items he will veto gives the Governor a chance to see which legislators back his agenda.
But the start of the fiscal year, July 1, is coming up fast. Most Governors usually sign the budget — and hand out their line-item budget vetoes — around Memorial Day. The Governor’s budget office has had plenty of time to go through the Appropriations Act, so it wouldn’t be surprising to see DeSantis act quickly once this week’s Special Session on property insurance is wrapped up.
Legislators as well as health care lobbyists, hospitals and other providers will soon know whether or not their budget priorities will make it to the finish line.
___
Thank you for reading, I welcome your feedback, questions and especially your tips. You can email me at [email protected] or call me at 850-251-2317.
— Extended again? —
It looks like the Joe Biden administration is prepared to extend the public health emergency associated with the COVID-19 pandemic for another 90 days — a move that means Florida will continue to receive extra money from the federal government.
The current public health emergency is scheduled to end in July, but the administration also promised to give states 60 days notice if it planned to end the emergency. That notice deadline passed last week. CNN and Bloomberg reported last week that administration officials plan to extend the emergency declaration because COVID-19 cases have been rising.

The extension of the public health emergency means people can continue to receive free tests, vaccines and treatments for COVID-19.
But for state legislators and budget analysts, another extension means the state will continue to receive an additional 6.2% increase in the amount of federal Medicaid dollars to help pay the costs of the health care safety net program for the poor, elderly and disabled. If the administration does go ahead with an extension, extra money will continue to flow to Florida for both the first and second quarters of the 2022-23 fiscal year.
But that additional federal assistance comes with a requirement that Florida cannot remove anyone from the Medicaid program so long as the public health emergency is in effect. As of April 30, Florida’s Medicaid enrollment topped 5.2 million people. Florida normally requires children ages 5-19 and certain adults to be determined eligible for Medicaid every six months.
— Abortion action? —
As anti-abortion groups in Florida begin to push for the Republican-controlled Legislature to enact more restrictions due to a looming U.S. Supreme Court decision, state health care regulators issued an emergency order shutting one of the few Panhandle abortion clinics following the facility’s alleged failure to comply with state laws.
The Agency for Health Care Administration issued the emergency order May 20 and alleges, among other things, that Integrity Medical Care, which operates as American Family Planning, did not report to the state that three of its patients were transferred to hospitals because they required advanced care.

AHCA alleges in the complaint that following an alleged second trimester abortion on March 23, one patient was transferred to a nearby hospital for emergency surgery. The patient required a total abdominal hysterectomy with bilateral salpingectomy and received ten units of blood.
A second patient need resuscitation and a transaction to replace “egregious loss of blood” following a May 5 abortion. The physician didn’t complete the abortion, with the surgeon noting cervical laceration and possible uterine rupture.
The state alleges that the physician performing the abortion directed the patient’s spouse to drive her to a hospital in Alabama even though care was available at a nearby hospital that the clinic had a transfer agreement with. The state alleges that it created an unnecessary delay in the patient receiving emergency care.
The clinic also got cited for failing to report the transfer of a patient to a hospital in 2021. Ultimately, the patient required repair of a uterine perforation, a colon resection, a colostomy, a sigmoidectomy, and a cystoscopy.
The U.S. Supreme Court appears poised to reverse Roe vs. Wade, the decision that struck down many state abortion laws, according to a draft opinion that was leaked earlier this month.
Florida recently passed a new law that bans all abortions after 15 weeks of pregnancy in anticipation that the high court would uphold a similar law enacted by Mississippi.
But the release of the draft opinion has led some anti-abortion leaders to advocate that Florida go further. Some have advocated for a measure that would block abortions after six weeks, or when a fetal heartbeat can be detected.
— Asked and (sometimes) answered —
Memorial Day is just around the corner, and the official start of summer is underway. But the days aren’t going to be lazy anytime soon for vendors planning on responding to the request for information (RFI) published May 6 by the Agency for Health Care Administration regarding Florida’s multi-billion dollar Medicaid managed care contracts. Responses are due by 5 p.m. on June 3.
To that end, AHCA provided answers to some of the 19 questions interested parties and health plans had timely submitted to the state regarding the RFI.
The agency said it “prefers” responses to have a minimum 11-point font and that it will not accept Adobe files. And, AHCA said, responding to the RFI doesn’t get vendors extra credit points that can be applied to their responses to the statewide Medicaid Managed Care re-procurement.
But not all questions sent to the state were answered. And sometimes AHCA’s responses didn’t answer the questions that were asked.
AHCA would not say whether it would be “reviewing” the performance bond contracts or whether it would be providing “transparency” into how administrative load costs are determined, which were from questions submitted by Molina Healthcare.
AHCA said the questions did “not address the subject matter” of the request for information and that they “will not be answered.”
The agency avoided directly answering some of the other questions.
Simply Healthcare Plans, Inc., for instance, said it was aware responses to the request for information were public record. The health plan asked AHCA about the timing of the release of the information. It wanted to know whether the agency would release the responses to the RFI prior to the upcoming procurement of the Statewide Medicaid Managed Care (SMMC) Program, or release responses after the reprocurement is finalized.
AHCA didn’t answer the question, responding instead, that “all RFI responses will be subject to public records request, in accordance with Chapter 119, Florida Statutes.” It then referred to RFI for additional details.
West Cocoa Pharmacy and Compounding asked AHCA whether it was “taking comments from the general public, providers and recipients“ on the RFI.
AHCA responded, “Yes, all providers, or interested providers, are welcome to reply.”
— Storm ready —
The statewide association that represents Florida’s nursing homes says it is helping nursing homes get ready for the looming hurricane season, a topic that has caused wrangling in the past between state regulators and the industry.
The Florida Health Care Association announced Friday that it recently hosted a hurricane preparedness webinar between its members, as well as the Agency for Health Care Administration and the Department of Health. The association also stated that nursing homes have reviewed their emergency plans, checked all their generators, restocked emergency supplies and developed plans to respond to power outages.
“Since we’re in the most hurricane-prone state, our nursing centers train and prepare throughout the year for hurricane season,” said Emmett Reed, CEO of the Florida Health Care Association in a statement. “The training and tools we offer to our members help ensure that nursing center residents and staff are ready for a disaster at any time.”
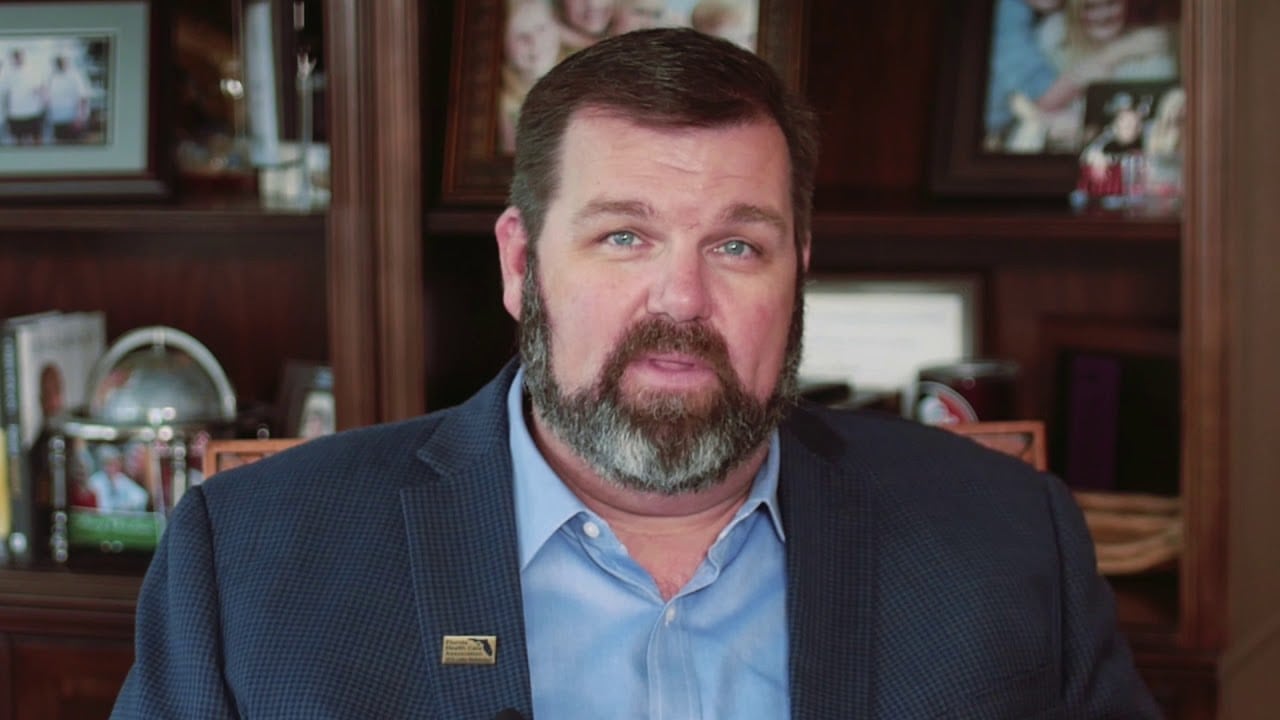
Twelve residents died in 2017 after a Hollywood nursing home lost power and could not run its air conditioning due to Hurricane Irma. A study released last November by a team of national health researchers found that there was an increase in mortality odds at Florida nursing homes following Hurricane Irma.
The state responded to the deaths by instituting mandatory rules for nursing homes that required either generators or access to generators. While emergency rules pushed by then-Gov. Rick Scott drew some legal challenges, the industry and the state reached an agreement on a state law that was adopted in 2018.
AHCA currently reports that 99.6% of assisted living facilities and 99% of nursing homes are in compliance with rules regarding generators and emergency power plans. FHCA says there is an emergency reporting system in place that keeps track of nursing homes’ needs and that providers have worked on emergency plans with local authorities regarding power in case there is an outage.
— RULES —
The Board of Pharmacy proposes amending Rule 64B16-26.1032 to update its application forms. More here.
The Board of Orthotists and Prosthetists proposes developing an amendment for Rule 64B14-5.002 for continuing education requirements and mandatory courses. More here.
The Board of Orthotists and Prosthetists proposes developing an amendment for Rule 64B14-7.001 to clarify definitions regarding its standard of practice. More here.
The Board of Nursing Home Administrators is proposing an amendment to Rule 64B10-12.0001 to update the text to remove the application for recertification from the fees. More here.
— ROSTER —
— Gov. DeSantis appointed Stacy Angier of Margate and Paul Tanner of Fort Lauderdale to the North Broward Hospital District board of commissioners. Angier is the principal at Abundant Life Christian Academy. She is a current board member for the Children’s Diagnostic and Treatment Center and the League of Christian Schools. She earned her bachelor’s degree from Miami Christian College and a master’s degree from Oral Roberts University. Tanner is the owner and founder of Las Olas Capital Advisors. He is a board member for the Urban League of Broward County and sits on the Investment Committee of Broward Community Foundation. He earned his bachelor’s degree in political science from Florida Atlantic University. The North Broward Hospital district operates as Broward Health.

— Marcia Young has been named the Chief Operating Officer of FoundCare, a federally qualified health center that has seven locations in Palm Beach County. Andy Antenor will serve as as Chief Financial Officer FoundCare offers low income individuals a medical home offering pediatric, adult, and geriatric primary care, chronic disease management, behavioral health services, dentistry, laboratory services, women’s health (including screening mammography), and an on-site pharmacy. FoundCare’s services are accessible through seven locations in Palm Beach County. Young has worked in health care for more than 30 years and received her master’s degree in health service administration from Nova Southeastern University. Antenor has a masters’ degree in business administration degree in finance and management from Barry University and master’s degree in forensic accounting from Florida Atlantic University.

— Deborah Hall, CHC, CFSA, CRMA, has been named the chief internal auditor at Broward Health. Hall has a Bachelor of Science in Business Administration from American International College in Springfield, Massachusetts. She has previously served as the compliance and privacy officer at Randolph Health in Asheboro, North Carolina; vice president, chief compliance and privacy officer, internal audit at the Healthcare District of Palm Beach County in West Palm Beach; and revenue cycle compliance and privacy officer at Sisters of Charity in Broomfield, Colorado.
— Weesam Khoury has been named the Deputy Chief of Staff at the Florida Department of Health.
— ICYMI —
In case you missed them, here is a recap of other critical health care policy stories covered in Florida Politics this past week.
— No. 3 in new cases: Florida recorded more than 55,000 new cases of COVID-19 in the week through Wednesday, the highest seven-day total seen since the winter 2022 surge was waning in early February. Florida’s latest case tally from the U.S. Centers for Disease Control and Prevention — 55,390 over seven days through Wednesday was one-third higher than the week before. Only California, with 77,000 cases, and New York, with 71,000, saw more new cases emerge during the week.
— Clueless: Democrats from the White House to Florida are continuing to go after Sen. Rick Scott and his “11-point plan to rescue America,” which proposes a five-year review of Social Security, Medicare and Medicaid and would require the poorest Americans to pay taxes. Members of the Florida Democratic Disability Caucus have joined the chorus of critics with caucus member and Seminole County Alison Holmes noting that the former Governor has “no clue.”

— Perfect storm: Hundreds of thousands of Florida residents losing their health insurance coverage, warned Florida Covering Kids & Families Program Director, Jodi Ray. Ray said Thursday that costs of health insurance premiums could soar by 53% for more than 2.5 million people if Congress does not make permanent the enhanced subsidies that were included in the American Rescue Plan. She also said when the public health emergency expires later this year that hundreds of thousands of Florida children are expected to no longer qualify for Medicaid. While many of them will qualify for a program called Florida KidCare, children often become uninsured during the transition between the two health care programs. Florida’s children are considered to be some of the most at risk of losing coverage.
— Curing cancer: Gov. DeSantis gave the public a brief insight into the cancer treatment journey that he and his wife, First Lady Casey DeSantis, traveled last year in her fight against breast cancer. The comments were made at a press conference called by the Governor to announce his support of the Legislature’s decision to spend an additional $37 million annually to fight cancer. The bump means the state will spend $100 million on cancer research at Moffitt Cancer Center, University of Miami Sylvester Comprehensive Cancer Center and University of Florida Health Cancer Center. DeSantis called the funding commitment a “really, really, big deal.”
— Boosting nursing education: Gov. DeSantis said Monday he will approve $125 million to help boost nursing education in the state. According to a Senate analysis, the Fiscal Year 2022-23 budget directs $125 million in nurse training in three different education areas of the budget: $20 million for workforce training; $59 million for state colleges; and $46 million for the state university system, which includes Florida’s public universities.
— FOR YOUR RADAR —
Aside from coverage by Florida Politics, these stories are worthy of your time.
—“Two state complaints filed against a Fort Lauderdale doctor. He says racism is involved” via David J. Neal of the Miami Herald — The Florida Department of Health has accused Fort Lauderdale Dr. Jeffrey Morgan of being a pill slinger and doing a Brazilian Butt Lift surgery at a Tampa clinic that wasn’t registered for that surgery. Morgan accused the Florida Department of Health of “making wildly fraudulent accusations” and of “hate bias” designed to end his career.
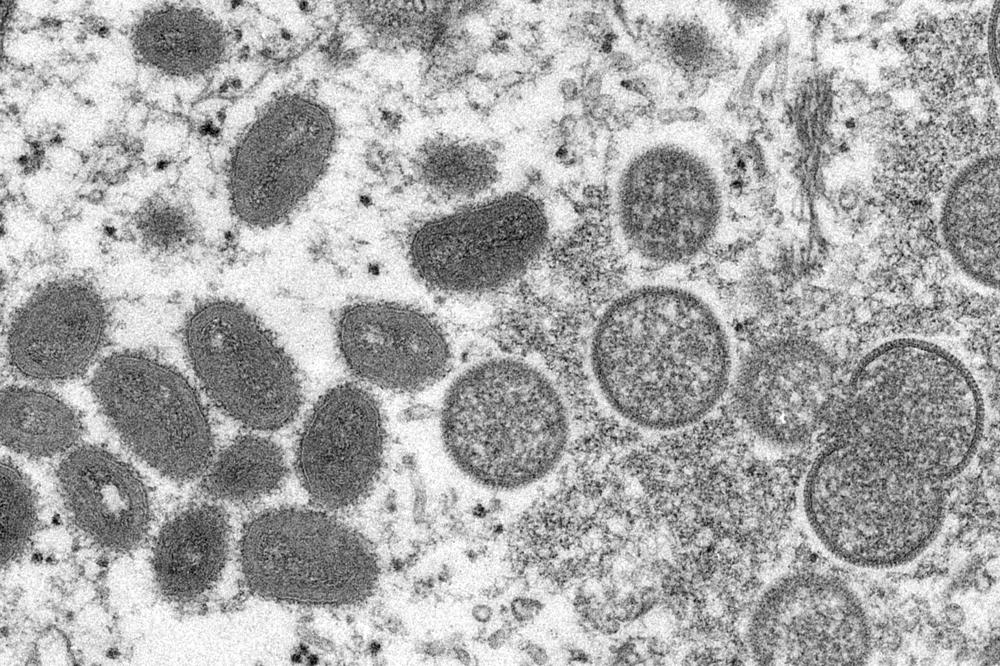
—“Monkeypox South Florida: Health officials investigate possible local case” via BocaNewsNow.com — The Florida Department of Health in Broward County is investigating what is described as a ”presumptive” case of monkeypox. Health officials released the following statement just after 3 p.m. on Sunday, May 22, 2022:
—”Two Tampa men sentenced in multimillion-dollar health care fraud scheme” via Julio Ochoa of WUSF — Two Tampa men have been sentenced to prison after being convicted in a multimillion-dollar health care fraud scheme. Peter Bolos, 44, was sentenced to 14 years in prison, while Michael Palso, 48, was sentenced to 33 months in prison. Both were also ordered to pay more than $24.6 million dollars each in restitution.
—”People who are making health care more fair: Four innovators are finding new solutions for the problem of injustice” via Julia Hotz of Scientific American — The world has never had better medicine, more knowledgeable doctors or stronger data on disease. But these benefits are not equally shared. To take one conspicuous example: two years of data from the Centers for Disease Control and Prevention show that Black, Hispanic and Native American people are significantly more likely to be hospitalized and die from COVID-19 than white people in the U.S. Health inequity includes the lack of access to appropriate care, the failure to address social factors that influence health, and the dangerous conditions that people in some neighborhoods endure. Achieving equity requires campaigns on all these fronts. These four health care champions — a data-digging epidemiologist, an activist midwife, a doctor who traded clinic work for community activism and a pollution-tracking entrepreneur — embody that effort.
—”How leaders at Salesforce, Zoom, and Best Buy are using technology to change health care” via Carmela Chirinos of Fortune Magazine — The pandemic gave patients more power than ever before, and millions of people are now taking charge of their health. For big companies, technology can help bridge surging new demands for primary and specialty care.
— LEFTOVERS —
— Seeking input: The Division of Workers’ Compensation is looking for “ideas and suggestions for topics” that should be addressed in an upcoming “Three Member Panel” report. The recommendations must address methods to improve the workers’ compensation health care delivery system. Health care providers, insurers and claims administrators can submit recommendations via email to Brittany O’Neil at [email protected]. Recommendations must be submitted by May 31.
— Certificate of Need: Sabal Palm Nursing and Rehab Center, LLC is transferring Certificate of Need #10641 to Riverview Nursing and Rehab Center, LLC to establish a new 67-bed community nursing home in Hillsborough County.
— Mental health month: Rep. Kathy Castor has filed legislation that would establish a new grant initiative at HHS to hire and retain mental health and substance use disorder care providers in schools. Care providers include counselors, psychologists, psychiatrists and social workers, among others. The Advancing Student Services In Schools Today (ASSIST) Act (H.R. 7672) includes a 90% increase in federal Medicaid matching funds to pay for these services, to incentivize these professionals to work in schools and retain them.
— Connected: The Affordable Connectivity Program, which connects lower income Americans with subsidized broadband internet has been expanded. Qualifying households at or below 200% of federal poverty guidelines, or that participate in anti-poverty measures like Medicaid or Supplemental Nutrition Assistance Program, are eligible for high-speed internet for no more than $30 a month. Find out more at getinternet.gov.
— PENCIL IT IN —
Monday
Happy birthday, Sen. Ana Maria Rodriguez.

Tuesday
Happy birthday, Rob Johnson, partner at The Mayernick Group.
2 p.m. The Florida First Responder Suicide Deterrence Task Force meets. Information at https://www.myflfamilies.com/suicideprevention.
2:30 p.m. The Florida Cybersecurity Advisory Council meets. University of North Florida, 12000 Alumni Dr., Jacksonville.
Wednesday
1 p.m. The FX Executive Steering Committee meets. Agency for Health Care Administration Conference Rooms A, B, and C. 2727 Mahan Drive, Building 3, Tallahassee.
Friday
9 a.m. The Board of Nursing Probable Cause Panel meets to discuss disciplinary cases. Call (888)-585-9008; participant code: 275112502. Agenda here
Saturday
Happy birthday Craig Waters, the former communications director at the Supreme Court of Florida.



